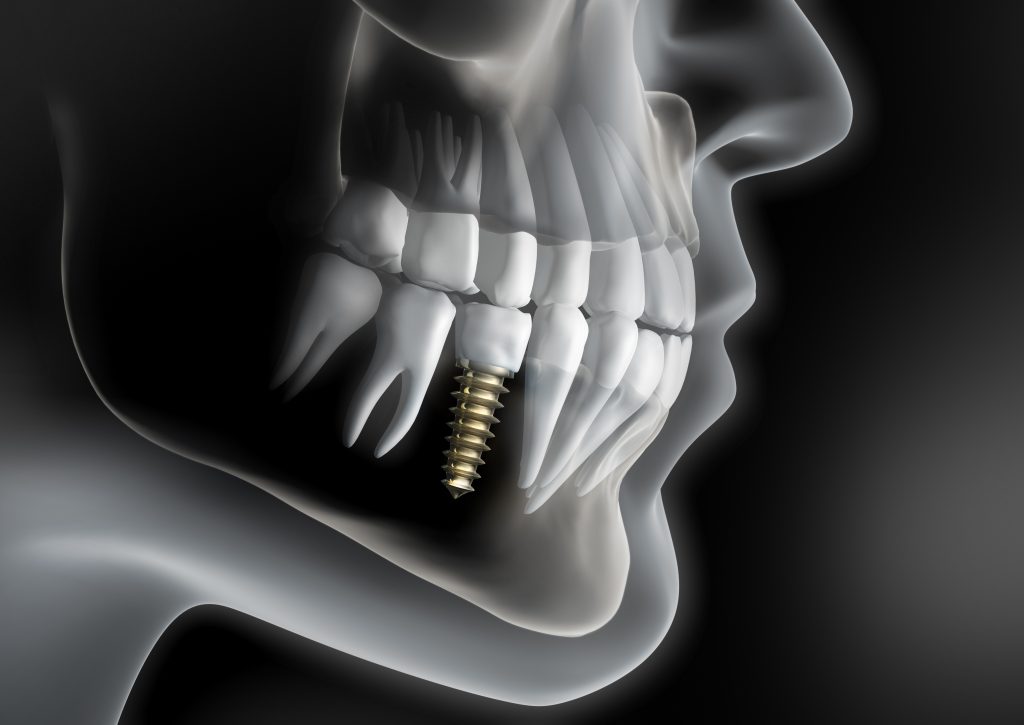
A dental implant is a treatment option to replace a missing tooth or teeth. It is a small titanium screw or cylinder that acts as a replacement for the root section of a missing tooth. Dental implants are placed within the upper or lower jaw bone in a minor surgical procedure and the bone fuses or osseointegrates with the titanium screw over a period of time. Artificial teeth can then be attached to the implant or implants once they have integrated into the bone. Dental implants can be used to support a number of dental prostheses, including crowns to replace single missing teeth, bridges to replace several adjacent missing teeth or overdentures to replace all missing teeth. Dental implant-supported teeth look, feel and function like natural teeth
Dental implants are one of the most significant advances in modern dentistry. They have changed the way people live. With them, people who have lost teeth are rediscovering the comfort and confidence to eat, speak, laugh, and enjoy life. If you feel embarrassed or uncomfortable about gaps, missing teeth, dentures that are loose or unexpectedly drop down or you are unable to chew properly, dental implants may be the solution for you.
Dental implants are intimately connected with the gum tissues and underlying bone in the mouth. Since periodontists are the dental specialists who specialize in precisely these areas, they are ideal members of a dental implant team. Not only do periodontists have experience working with other dental professionals, they also have the special knowledge, training and facilities that you need to have teeth that look and feel just like your own. Your periodontist will work with your dentist to replace your missing tooth or teeth.
Dental implants are suitable for almost anyone who has lost one or more teeth and would like to restore their appearance or chewing ability. The ideal candidate for a dental implant is in good general and oral health and the best candidates have healthy gum tissues that are free of Periodontal disease or other infections. Adequate bone in your jaw is needed to support a dental implant. However, if adequate bone is not present then additional augmentation procedures, such as the use of bone grafting , can usually be performed to create the volume of bone required to place a dental implant. Whilst dental implants are far and away the best treatment option to replace missing teeth, they are not for everyone. Some people, such as those who suffer from uncontrolled diabetes, untreated periodontal disease, alcoholism, bleeding disorders or immunocompromised conditions do not make good candidates for dental implants. Currently, certain medications such as the use of intravenous bisphosphonates also preclude the use of dental implants. Smoking is also an important consideration, because smokers heal less efficiently than non-smokers and are more likely to experience unsuccessful integration of their implants. Quitting smoking will significantly increase your chances of successful implant therapy.
It is also not advisable for people below the age of 18 to have dental implants as their jaw bone growth has not fully finished.
Short version
In its most basic form, the placement of a dental implant requires placement of a titanium screw into the bone during a minor surgical procedure. Following a period of time, and once the implant has completely integrated into the bone, the dental implant is then uncovered and “loaded” with the tooth it is designed to replace.
For a more detailed explanation of the implant placement procedure please read on below.
Long version
A dental implant-retained restoration is not a single one-stage procedure as biological healing cannot be rushed. It can take 4-9 months, depending on the case, for implant treatment to be completed. There is generally a surgical phase followed by a restorative phase.
If the tooth to be extracted is still present in the mouth then it is important that it is extracted as ‘atraumatically’ as possible. This is so that as much bone as possible is preserved for future implant placement. Sometimes, and depending on the case, a socket preservation procedure may be required at the time of tooth extraction in order to ensure adequate bone for implant placement later on.
Following extraction, it is necessary to wait for a period of time in order to ensure that natural bone remodelling has finished in the area that the tooth has been extracted. The only reason why bone is present in the jaws is to anchor the teeth in and once a tooth is extracted bone shrinkage or atrophy occurs in the area. This amount of bone atrophy varies from person to person. Once most of the remodelling has occurred, usually a period of three months following tooth extraction, a CT scan or cone beam scan is taken of the area. This three-dimensional radiographic scan is useful in assessing the bony anatomy present and the information gathered from the scan is evaluated on a computer program. The location of critical structures such as the mandibular nerve or the floor maxillary sinus needs to be identified and the shape and volume of the bone present needs to be assessed. This information assists in determining the proper orientation of the dental implants to be placed and careful and detailed planning is then undertaken for implant placement surgery.
Dental implant surgery usually occurs in two phases. Implant surgery is considered to be a routine procedure and can be comfortably performed under local anaesthesia in the dental surgery. In fact, it is often less traumatic than extraction of a tooth. Stage 1 surgery involves making an incision in the gums and folding it back to expose the underlying bone. A channel is drilled into the bone, taking care to ensure that it is at the correct depth and angulation. Digital radiographs are often used to guide the orientation of the channel. The channel is then gradually widened to the correct diameter before a dental implant is carefully torqued in. A cover screw is then placed on the implant and the gums are then stitched back into position so that the implant is covered. If any bone grafting to replace minor bone loss is required then this can be done at this stage concurrently with implant placement.
Second stage surgery involves uncovering the top of the implant and assessing whether it has integrated into the bone. It is usually performed three months after Stage 1 surgery. A ‘healing cap’ is then placed on the implant and this healing cap ends up protruding through the gums which then heal around it.
Following a period of 4-6 weeks after Stage 2 surgery, your dentist or prosthodontist can start construction of a crown or bridge that will be supported on the implants. This usually involves taking a mould or an impression of the area and sending it to a dental lab for construction of the porcelain or metal tooth. An abutment or connector is then attached to the implant before the tooth or bridge is then either screwed or cemented onto the implants.
Several variations on the above protocol are possible. Sometimes, if conditions are conducive, a healing cap is placed straight away and a second stage surgery is not required. In other selected cases, dental implants can be placed earlier than 3 months following tooth extraction and, very occasionally in a suitable patient, a dental implant can be placed immediately following tooth extraction.
Sometimes, if there has been severe bone loss following tooth extraction and there isn’t enough bone to anchor a dental implant then a bone grafting procedure may need to be performed separately prior to dental implant placement.
At all stages of implant treatment before the final crown or bridge is placed in, a temporary denture or temporary bridge can be worn to have the appearance of a tooth in the area where tooth loss has occurred.
After dental implant treatment is completed, it is essential to attend for regular follow-up appointments with your dentist or periodontist, so that the implants can be clinically assessed and steps can be taken to prevent any complications at an early stage.
During a consultation appointment, the patient’s complete medical and dental histories will be reviewed in order to ensure that they are a good candidate for dental implant treatment. A thorough oral examination, including a periodontal assessment, will then be carried out in order to ensure that there is no infection present in the mouth as this will increase the chances of implant failure. Finally, an assessment of the site of the missing tooth will be undertaken to assess the feasibility of implant placement. This will include assessment of radiographic imaging. If the missing tooth has been extracted for over 3 months then a CT or cone beam scan of the area will be required prior to the consultation appointment and this should be arranged for prior to the consultation appointment. If it has been less than 3 months following tooth extraction or if the tooth has yet to be extracted then the periodontist can arrange for the CT or cone beam scan after the initial consultation appointment. The periodontist will also explain in detail the procedures involved in dental implant placement as well as the advantages, disadvantages and any potential risks involved with implant treatment. Following this, the timings and costings of the patient’s treatment plan will be discussed with the patient at reception before appointments for appropriate treatment can be booked in.
There are generally 4 treatment options to replace a missing tooth.
1. Do nothing
Needless to mention, doing nothing to replace a front tooth is not a treatment option that would be acceptable to most people as there are often embarrassment issues associated with smiling and speaking. If a non-visible back tooth was missing then, an individual may not feel the need for a replacement as there are no issues when smiling and there may be adequate teeth left to chew with. However, the consequences of doing nothing means that the teeth on either side of the gap often drift and the teeth on the other set of jaws overerupt in the area of the missing tooth, and this can have functional consequences for a person’s bite.
2. Removable dentures
Traditional dentures have the advantage of being simpler to construct and they are also the least costly treatment option. However, they are far less tolerable and offer far inferior chewing ability than other treatment options, so much so that people often have to sacrifice what they would like to eat for what their dentures can allow them to chew. Removable dentures often have other issues associated with them such as social embarrassment when kissing, speech difficulties and difficulty when chewing. Most people also do not like the idea of having something that must be taken out at night and soaked in a glass of water. Finally, the bone underneath a removable denture will continue to resorb over time and either a reline of the existing denture or new dentures may be required after a period of time.
3. Bridges
A bridge is a fixed treatment option that relies on the teeth adjacent to the missing tooth for support. However, it is necessary to significantly cut back and drill into the adjacent teeth to make space for the supports. This then compromises the health of the adjacent teeth for the sake of replacing one missing tooth. Further, if there are two or more missing adjacent teeth then a bridge is often not a viable treatment option as long spans of missing teeth cannot be restored with a bridge. With the advent of dental implants, a bridge is no longer considered to be a good treatment option if there are two intact teeth on either side of the tooth to be replaced.
4. Dental implants
Dental implants have the disadvantage of being the most expensive treatment option. Further, treatment to replace a missing tooth cannot usually be completed in a short period of time. However, they are also the gold standard treatment option. Whilst nothing can replace a natural tooth perfectly, dental implants are the treatment option that most closely mimic the original tooth that was lost. They look, feel and function more natural than other treatment options and are also more secure. The adjacent teeth are not damaged or cut in any way and placement of a dental implant will prevent further bone loss in the area. If several teeth are missing then it is possible to place various configurations of implants so that implant-supported fixed bridges or even secure implant-retained dentures can be placed.
If one tooth is missing then one dental implant will be required to replace it. If two adjacent teeth are missing then most often two dental implants will be required to be replace them. If three or more adjacent teeth are missing then it is usually possible to restore the missing teeth with less implants than the number of teeth missing.
The procedure of dental implant surgery is completely pain free thanks to the administration of local anaesthetic prior to the procedure. Most people report that they were much more comfortable following the procedure than they had anticipated.As with any surgical procedure there will be some swelling and discomfort in the area for a couple of days following implant surgery. Painkillers will be prescribed to you following implant surgery that will help minimize any discomfort that you may experience.
Although every effort is always made to ensure successful integration of a dental implant, implants do sometimes fail due to the biological nature of the healing process. Early implant failure occurs when the implant has not successfully attached or integrated to the bone due to infection around the implant or due to excessive micromovement of the implant during the healing phase. This failure is usually evident at second stage surgery when the integration of the implant is tested. If this occurs, the failed implant is unscrewed, the bone left to heal for a while and a new implant placed. At Townsville Periodontics and Dental Implants,this is done at no further charge to the patient as long as all post-operative instructions have been adhered to, the patient is a non-smoker and the patient attends for regular post-operative recall appointments. Late implant failure can occur up to several years after implant placement. The most likely cause of late failure is inadequate oral hygiene. If tooth cleaning is poor, bacteria will build up on the implant surface and cause inflammation of the gums and bone surrounding the implant. This can lead to bone loss around the implant. Eventually, the implant loses its anchorage in the bone and becomes loose. For this reason it is vital that good oral hygiene practices are maintained around an implant and that a patient attends for regular recall appointments. Smoking can also lead to a higher rate of late implant failure.
Dental implants have some of the highest success rates for any procedure that can be performed in dentistry today. They have successfully been used for many decades and in most studies 95% of dental implants last for at least 5 years, but most are likely to have a much longer life. However, the exact lifespan of a single dental implant is impossible to predict. The longevity of dental implants can be maximized by maintaining excellent oral hygiene, not smoking and by attending regular recall visits for careful inspection of the implants. This will enable any potential problems to be dealt with promptly before they threaten the stability of the implant. In effect, dental implants are like your own teeth and will require the same care.The success rate of dental implants also depends on the location of the jaw where the implants are placed. The front part of the lower jaw has a higher success rate than the back part of the upper jaw. However, even here the success rate is generally over 90%. If you smoke, the chances of success drop by at least 10%.
Following implant surgery, it is normal to experience varying degrees of swelling and soreness. Sometimes there can also be some minor bruising in the area. Complications following surgery may also occur although every step is always taken to avoid these via thorough planning and a careful surgery technique. These may include:
At no stage of implant treatment will you have to live without a tooth in place of the one that has been lost. If a front tooth is to be extracted then a temporary denture is constructed prior to tooth extraction. This temporary denture is then inserted into the mouth immediately following tooth extraction and lends the appearance of a tooth being present in the area. The temporary denture will also be present during the healing period after the implant has been placed in. It will be slightly adjusted so that it only exerts minimal pressure in the area before being placed in the mouth again.In some circumstances it may also be possible to anchor a temporary crown to the dental implant immediately following implant placement.
Bone grafts are carried out to increase the width and height of the jawbone at the intended implant site. This is essential in cases where there is inadequate volume of bone present to successfully anchor in a dental implant. Bone grafting can be performed by either using your own bone (which is harvested from another site such as the corner of the lower jaw) or by using synthetic or animal-derived bone substitutes. These grafts act as scaffolding for your own bone cells to migrate into the area and form new natural bone so that the bone grafts are replaced with new bone over time.Whenever bone grafting is performed, it is usually in conjunction with the use of a barrier membrane. The barrier membrane is used to cover the bone graft as well as the area where bone has been lost. This then aids in promoting new bone formation because it blocks infiltration from other types of cells such as those present on the gum surface or the underlying connective tissues, which are normally faster at migrating and proliferating. The barrier membrane used will disintegrate over time or may need to be removed at a later date depending on the type of membrane used.
The cost of dental implant placement varies from case to case depending on the number of implants and their configuration as well as whether any additional procedures such as bone grafting or temporary tooth replacements are needed. These costs can more accurately be judged during a consultation appointment after a thorough examination is performed and all the required information is obtainedIt is also important to be aware that there will be a cost for surgical placement of the dental implant/s as well as a cost for the placement of the tooth or teeth that are to be supported by the implant/s. It would be advisable that before undertaking implant treatment that you be aware of all costs involved in advance.
Just as is the case around natural teeth, dental implants can be susceptible to infections in the gums if oral hygiene is poor. As such, it is important to care for and clean you dental implants like you do your natural teeth. Twice daily brushing, flossing and/or using interproximal brushes around a dental implant are essential.Regular dental check-ups are also necessary and it is also important to have an X-ray taken of your dental implant occasionally in order to ascertain that the bone levels around it remain healthy.